Treatment of Super-Eruption Secondary to Anterior Wear
Considerations for crown lengthening versus orthodontic intrusion
Salvatore Lotardo, DDS, AAACD
With the prevalence of bruxism and erosion, management of super-eruption secondary to anterior wear has become a more common challenge. As demand grows for comprehensive and cosmetic solutions for these cases, clinicians are faced with complex treatment decisions. It is often the esthetic issues that drive the patient to seek care, making esthetics essential for the success of the case.
A successful outcome is predicated on identifying the etiology of the current condition and understanding the factors influencing the long-term predictability of treatment. A comprehensive approach and sound occlusal strategy are paramount. Once the clinician has determined a course of treatment, a plan for handling the esthetic challenges in the smile zone, including short teeth, excessive gingival display, and uneven gingival margins, must be developed.
The diagnosis of super-eruption secondary to anterior wear needs to be established, ruling out other conditions such as altered passive eruption, which could have different treatment modalities. There are several options in cases where the occlusion and posterior teeth have been addressed, or when the clinician is treating anterior teeth in an otherwise functional, low-risk occlusion and not substantially changing the present occlusion via increasing vertical dimension or anteroposterior relations. These options include crown lengthening, orthodontic intrusion, or a combination of both—each of which may also include various restorative combination procedures as well.
When upper anterior teeth are worn, any of the following may occur: (1) upper teeth super-erupt; (2) lower teeth super-erupt; (3) both upper and lower teeth super-erupt; or (4) something—tongue thrust or habit—prevents the worn teeth from erupting. When the upper teeth super-erupt, the worn teeth and the periodontium move incisally together, creating a lower gingival margin for those teeth.1 The initial goal is to first determine the desired incisal edge position, followed by the incisal length. This is accomplished following principles of smile design, many of which use the maxillary incisal edge position as the starting point. Once incisal edge position and central incisor length are determined, the corrected gingival margin follows suit, as set by the latter. To clinically establish the corrected gingival height, there are factors to consider that will allow for the least invasive and most effective treatment.
Considerations for Treatment Selection
The following are the findings and their implications for treatment. Each finding tends to favor either crown lengthening or orthodontic intrusion. Consideration of these factors will help to formulate the best treatment plan decision.
Presence of Misaligned Teeth or General Malocclusions
Correction of other orthodontic issues as an additional benefit to the treatment of super-erupted teeth will improve overall outcomes and be an additional motivational factor for patient acceptance. In restorative cases, orthodontic correction leads to more conservative preparations. Therefore, in these cases, intrusion is favored over crown lengthening. Of note is the risk of black triangles after orthodontic treatment, especially on rotated or crossed anterior teeth in adult patients.2 Patients need to be made aware of this risk, and the need for additional treatment should be a factor. If the plan is to intrude crossed incisors, the starting position of the papilla—and hence the new contact point—may need to be adjusted to eliminate the black triangle.
Crown-Root Ratio
Crown-to-root ratios of less than 1:1 are considered by some to be a contraindication for use in crown-and-bridge treatment.3,4 If similar guidelines are used and less favorable crown-to-root ratios preclude crown lengthening, orthodontic intrusion may be the only option for repositioning gingival margins.
Restorative Treatment Needs
If restorations are needed for esthetic, caries, or structural purposes, the next decision will be the type of restorations required. For porcelain veneers, crown lengthening may mean cervical margins don’t end on enamel, resulting in a higher prevalence of marginal leakage and poorer bond strengths, whereas intrusion moves the cementoenamel junction (CEJ) apically and preserves the porcelain-to-enamel bond cervically.5,6 Full-coverage restorations, if planned, may require circumferential osseous crown lengthening, which is a more invasive procedure than that required for facial gingival repositioning only. If the remaining amount of tooth structure left after intrusion will be insufficient to retain a restoration, crown lengthening would be indicated.
Periodontal Health
Elimination of pockets and establishment of gingival health with periodontal therapy alone may result in the desired marginal position, negating the need for crown lengthening. Periodontal surgery to normalize the pocket and obtain optimal health prior to restorative treatment also allows for more predictable gingival margin stability after restorative insertion.7 Orthodontic treatment should not be started on patients with active periodontal disease. Once the periodontal health is established, orthodontic treatment can be done if gingival discrepancies persist beyond the periodontal therapy.8
Position of the Papilla
The height of the papilla should occupy the gingival portion below the contact point, which lies at the halfway point of the tooth length for a central incisor.9,10 If the tip of the papilla/contact point is nearer to the incisal, buccal crown lengthening could result in an elongated papilla and poor contact position. Intrusion would be more effective at correction, as the papilla and contact point will be moved more gingival as teeth are intruded. The apparent contact dimension for central incisors is 50%, meaning the height of the papilla is equal to 50% of the overall length of the central incisor; this ratio should be the goal and a consideration for the treatment modality that will best accomplish it.11,12
Tooth Shape
Triangular or tapered teeth are narrower cervically. This shape becomes more exaggerated as these teeth super-erupt, making restorations with ideal interproximal emergence profiles more challenging after crown lengthening. Alternatively, intruding these teeth will place the wider mesial distal dimension back into a more favorable esthetic position.
Tooth Inclination (Torque)
Retroclined teeth needing restorations are ideal for additive-only, minimally invasive dentistry. If intrusion is needed, there are orthodontic techniques that maintain the current torque and therefore keep the teeth in a retroclined position. If there is wear on the lingual as well as incisal, a restricted envelope of function may exist. In that case, intruding the teeth and correcting the torque can create needed overjet and space for full-coverage restorations. For proclined teeth, correcting the torque improves esthetics and is vital for preserving tooth structure if restorations are needed. Even when restorations are used to improve or mask proclination, the emergence profile is often compromised. The torque can be corrected or manipulated during the intrusion without significantly adding to the overall length of treatment.
Black Triangles
The complete or partial loss of the papilla may not be predictably corrected by orthodontics alone, and, as previously stated, “untangling” crowded teeth may actually lead to or worsen a black triangle. Tarnow’s crest-to-contact-point findings make it possible to determine the probability of papilla loss or presence.13 By using that information in conjunction with a smile design, the clinician can devise a treatment plan to best deal with this issue. From the smile design, it has been determined where to place the gingival margins and contact points. If intrusion is being considered, the future crest position caused by the intrusion must be accounted for. Because a crest more apically positioned presents more of a challenge in terms of preserving papilla volume, this situation favors crown lengthening, whereby the incisal position of the papilla remains. Osseous crown lengthening combined with restorations may allow more flexibility for the creation of a more favorable contact-to-crest dimension.
Midline Discrepancy/Cant
There are limits to how much a cant or a midline discrepancy can be masked or corrected with restorations only.14 Consider correcting concomitantly with orthodontic intrusion.
Gingival Biotype
Thinner, higher scalloped biotypes have a higher incidence of recession after periodontal procedures and restorations. If this were a concern, intrusion would be favored.15
Attached Gingiva
If there was not an adequate band of attached gingiva apical to the teeth in question, intrusion would be favored.
Minimally Invasive Dentistry
In the end, the least invasive treatment option that will achieve the desired results most predictably is the goal.
Case Presentation 1
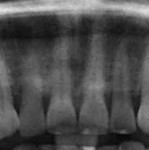
A 36-year-old woman presented with a chief complaint of short front teeth, gummy smile, and space behind her upper left canine (Figure 1 through Figure 4). After a comprehensive examination, the following findings, diagnosis, and treatment plan recommendations were reviewed with the patient.
General Findings
Upper incisal edge wear (teeth Nos. 8 and 9) with shortened clinical crowns, no wear of the posterior teeth, and mild wear and crowding of the lower incisors were observed. The TMJ was within normal limits. Gingival margins were uneven, but there was an otherwise healthy periodontium without significant pocketing. The occlusion was class 1 with a small diastema between Nos. 11 and 12.
Diagnosis and Smile Design
The diagnosis of super-eruption secondary to wear was established by the findings of short teeth (less than the typical length of 10 mm to 11 mm for central incisors), incisal wear, and incisally stepped gingival margins.16 Altered passive eruption could be ruled out by the detection of the CEJ within the sulcus with an explorer, confirming that the entire dentogingival complex migrated incisally during the super-eruption.17,18 Most smile design analyses are conducted by working through a checklist to identify deficiencies in an organized approach, ultimately leading to a vision of the final design. For this case, the AACD’s Global-Macro-Pink-Micro concept was used to properly determine the new incisal edge position, tooth proportions, and gingival heights and contours.19 A smile design software program (Smile Designer Pro, Tasty Tech, www.smiledesignerpro.com) was used to visualize the proposed changes and serve as the author’s blueprint. This blueprint could also be used for laboratory and specialist communication and patient education.
Treatment Planning
Once the goal central incisal edge position was determined to be 1 mm incisally from the current one, a 76% width-to-height ratio placed the gingival margin 3 mm apical to the current one, increasing the overall length of the centrals from 7 mm to 11 mm (Figure 5). This additional length would satisfy her complaint of short teeth and improve her gummy smile. Because the occlusion was otherwise functional, only the anterior maxillary teeth required treatment. To accomplish the goals of the smile design, a combination of orthodontic intrusion and crown lengthening followed by composite restorations would provide the best outcome.
Treatment Discussion
The concepts regarding these case types, as described earlier, were used to help select this treatment decision. By using orthodontics to intrude the centrals 2 mm and crown lengthen the remaining 1 mm, the gingival margins were repositioned 3 mm apically without the need for any restorations that would have margins ending on cementum while allowing for a less invasive non-osseous surgery. Without intrusion, the papilla would have ended up occupying 75% of the overall length of the tooth, a departure from ideal. Intrusion would also make it possible to correct the retrusive crown torque, creating added overjet with a less restricted bite and an opportunity to close the diastema while the arch was bracketed. Aligning the lower teeth during treatment additionally motivated the patient during treatment.
Treatment Phase
The treatment option of limited orthodontics including intrusion followed by soft-tissue–only crown lengthening was presented and the patient, understanding the advantages of this approach, consented. Orthodontic brackets were bonded to the upper and lower teeth, and over the course of 6 months, teeth were aligned, spaces were closed, and teeth Nos. 8 and 9 were intruded 2 mm (Figure 6). The brackets were removed, and overlay retainers were fabricated. The patient decided to incorporate home bleaching 2 weeks prior to starting the next phase of treatment. In preparation for crown lengthening, models, photographs, and designs were used to create a new diagnostic wax-up. Presurgical periodontal probing of 2 mm to 3 mm on the facials of the maxillary anterior teeth confirmed that the remaining crown lengthening could be accomplished using a soft-tissue–only diode laser (ezLase™, Biolase, www.biolase.com). During crown lengthening, the clinician used a lingual putty matrix made from the diagnostic wax-up and a composite-layering technique blending incisal, dentin, and enamel shades to obtain the ideal incisal length position for teeth Nos. 8 and 9. Simultaneously, minor imperfections on adjacent teeth were restored (Figure 7).20 When the patient approved the final results, a new overlay retainer was fabricated. At 3 months, the patient returned for follow-up and photographs. She reported no issues and loved her new smile (Figure 8 and Figure 9).
Case Presentation 2
A 42-year-old woman presented with a chief complaint of short-looking, yellow teeth (Figure 10 through Figure 12). A comprehensive examination was completed and the following findings, diagnosis, and treatment plan recommendations were reviewed with the patient.
General Findings
Short teeth and wear limited to anterior teeth were observed. Central incisors Nos. 8 and 9 were affected the most with severe super-eruption, as revealed by the uneven gingival margins.
Diagnosis and Smile Design
Super-eruption secondary to anterior wear was confirmed, and the smile design analysis was completed as described earlier. The analysis indicated that lengthening the current incisal edge position 1 mm and repositioning the gingival margin apically 4 mm for a new central incisor length of 10 mm, would be optimal. Also noted was the deficient development of the buccal corridors and excess gingival display on full smile.
Treatment Discussion
Crown lengthening to accomplish the new gingival position would require osseous surgery (potentially circumferential for full coverage, if indicated). The necessary restorations would be mostly on dentin, resulting in lower bond strengths if adhesively retained veneers were being considered. Crown-to-root ratios were within range for crown lengthening but they were approaching guideline limits. Orthodontic intrusion would negate the need for such aggressive surgery while preserving enamel and allowing more material and restorative options. With orthodontics, the retroclined centrals could be improved, but the retention on the remaining tooth structure after intrusion would be compromised. The papilla position that was near the incisal embrasure could best be moved into ideal position with intrusion. Based on the shape of the non-super-erupted teeth, the central tooth shape was likely triangular, and without intrusion, this would be even more challenging to restore.
Treatment
A combination of orthodontic intrusion and crown lengthening to maximize the benefits of each approach, followed by porcelain veneers on teeth Nos. 4 through 13, was presented to the patient. She refused orthodontic treatment and accepted an alternative plan of using crown lengthening and veneers on teeth Nos. 6 through 11. The gingival display beyond the centrals and the buccal corridor were not concerns for her.
Before starting treatment, mounted models, photographs, facebow (Kois Dento-Facial Analyzer, Panadent, www.panadent.com), and a smile design were sent to the laboratory for fabrication of a diagnostic wax-up, putty matrix, and surgical guide. Osseous crown lengthening was performed on teeth Nos. 8 and 9. Using a matrix-guided gingivectomy, this was followed by the use of an ostectomy technique to establish a new biological width with ideal gingival margin positions. After 6 weeks of healing (Figure 13), the patient returned for veneer preparation. The teeth were prepared for feldspathic porcelain veneers. Minor gingival zenith discrepancies were corrected using a diode laser. Final impressions, bite registration, and a second facebow relation were taken. The patient selected shade OM2 (VITA 3D-Master Linearguide, VITA North America, www.vitanorthamerica.com), and the preparation shade, ND2 (IPS Natural Die Material, Ivoclar Vivadent, www.ivoclarvivadent.com). All records were sent to the laboratory with a detailed prescription. Provisionals were made using a bleach shade bisacryl. The patient returned for final cementation and the shade and fit were verified. The patient approved the esthetics, and the veneers were bonded using translucent resin cement. The margins were finished and polished. Occlusion was checked in centric occlusion, lateral excursions, and protrusive. At the 4-week postoperative appointment, the case was evaluated and photographed (Figure 14). The patient was very satisfied and reported no sensitivity or functional issues (Figure 15).
Conclusion
Meeting the expectations of patients who are seeking esthetic improvements begins with excellent communication skills and knowledge of smile design principles. In cases where there are multiple treatment options, such as super-eruption secondary to wear in the smile zone, it is essential to understand the pertinent findings and how they affect treatment decisions and outcomes. When considering crown lengthening or orthodontic intrusion, it is important to know how each may impact the results, so the clinician should strive for excellence responsibly.
Disclosure
Salvatore Lotardo, DDS, AAACD, has no relevant financial relationships to disclose.
References
1. Spear F. A patient with severe wear on the anterior teeth and minimal wear on the posterior teeth. J Am Dent Assoc. 2008;139(10):1399-1403.
2. Sharma AA, Park JH. Esthetic considerations in interdental papilla: remediation and regeneration. J Esthet Restor Dent. 2010;22(1):18-28.
3. Grossmann Y, Sadan A. The prosthodontic concept of crown-to-root ratio: a review of the literature. J Prosthet Dent. 2005;93(6):559-562.
4. Penny RE, Kraal JH. Crown-to-root ratio: its significance in restorative dentistry. J Prosthet Dent. 1979;42(1):34-38.
5. Friedman MJ. Porcelain veneer restorations: a clinician’s opinion about a disturbing trend. J Esthet Restor Dent. 2001;13(5):318-327.
6. Decurcio RA. A harmonious smile. Journal of Cosmetic Dentistry. 2015;31(2):24-34.
7. Goldberg PV, Higginbottom FL, Wilson TG. Periodontal considerations in restorative and implant therapy. Periodontol 2000. 2001;25(1): 100-109.
8. Nanda R. Biomechanics and Esthetic Strategies in Clinical Orthodontics. St. Louis: Elsevier Saunders; 2005;18:560-581.
9. Kokich VG. Esthetics: the orthodontic-periodontic restorative connection. Seminars in Orthodontics. 1996;2(1):21-30.
10. Raj VJ. Esthetic paradigms in the interdisciplinary management of maxillary anterior dentition-a review. Esthet Restor Dent. 2013;25(5):295-304.
11. Robbins JW. Sequencing crown lengthening and orthodontic treatment. Inside Dentistry. 2010;6(5):54-57.
12. Morley J, Eubank J. Macroesthetic elements of smile design. J Am Dent Assoc. 2001;132(1):39-45.
13. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
14. Spear F. The esthetic management of dental midline problems with restorative dentistry. Compend Contin Educ Dent. 1999;20(10):912-914, 916, 918.
15. Tao J, Wu Y, Chen J, Su J. A follow-up study of up to 5 years of metal-ceramic crowns in maxillary central incisors for different gingival biotypes. Int J Periodontics Restorative Dent. 2014;34(5):85-92.
16. Gillen RJ, Schwartz RS, Hilton TJ, Evans DB. An analysis of selected normative tooth proportions. Int J Prosthodont. 1994;7(5):410-417.
17. Spear F. Using margin placement to achieve the best anterior restorative esthetics. J Am Dent Assoc. 2009; 140(7):920-926.
18. Bellamy LJ, Kokich VG, Weissman JA. Using orthodontic intrusion of abraded incisors to facilitate restoration: the technique’s effects on alveolar bone level and root length. J Am Dent Assoc. 2008;139 (6):725-733.
19. American Academy of Cosmetic Dentistry. A guide to Accreditation Criteria. Madison, WI: American Academy of Cosmetic Dentistry; 2014: 1-58.
20. Fahl N Jr. Mastering composite artistry to create anterior masterpieces-part 1. Journal of Cosmetic Dentistry. 2010;26(3):56-68.
Salvatore Lotardo, DDS, AAACD
American Board of Cosmetic Dentistry American Academy of Cosmetic Dentistry
Private Practice
Nesconset, New York