Surgical and Prosthetic Treatment of a Failed Maxillary Central Incisor
Immediate implant placement is a key to success
Robert A. Levine, DDS, FCPP, FISPPS
An esthetic zone implant restoration can be a complex, technique-sensitive procedure that frequently requires a collaborative effort. The case presented demonstrates immediate placement of a Bone Level Tapered (BLT) Roxolid® SLActive® implant (Straumann, www.straumann.us) to replace a maxillary central incisor. In addition to comprehensive case planning, the case entailed the use of an anatomically correct surgical guide, hard- (bone grafting of the buccal gap) and soft-tissue grafting (palatal connective tissue graft), and soft-tissue sculpting in the provisional phase.
Case Presentation
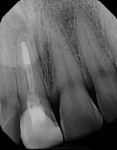
A healthy 26-year-old, non-smoking man (ASA 1) presented in November 2014 complaining chiefly of discomfort apically in the area of tooth No. 8, which had a prior root canal treatment resulting from a traumatic event to the face (Figure 1 through Figure 3). A full-mouth periodontal examination revealed minimal to no bleeding on probing depths greater than 3 mm. The patient was aware that No. 8 was hopeless due to a chronic periapical lesion and was interested in permanent tooth replacement. He presented with high esthetic expectations, a medium lip line and gingival biotype, and slightly triangular-shaped maxillary anterior teeth (Table 1).1-4
Treatment Plan
The comprehensive team treatment plan discussed with the patient was based on clinical and radiographic (including maxillary CT scans)5 examinations and comprised of several components. First, mounted study models were used with final restoration consultation among the author and restorative dentist for an anatomically correct maxillary surgical guide and a transitional Essix appliance for replacement of tooth No. 8. Then, surgical extraction of No. 8 would occur with evaluation for either immediate implant placement with hard- and soft-tissue reconstruction or ridge preservation with implant placement delayed for 3 to 4 months. The decision would be made after tooth extraction and 3-dimensional (3D) evaluation of the socket after full debridement of the apical lesion as well as insertion torque values.
Then, a screw-retained provisional for No. 8 would sculpt soft tissues and act as the “blueprint” for the final restoration. The patient would wear the provisional for 6 to 8 weeks, at which time the clinicians would reevaluate it for any modifications needed. Finally, upon establishing favorable soft-tissue scalloping and contours, a single crown would be completed for No. 8.
Treatment of Site No. 8 With Bone-Level Tapered Implant
The patient was medicated prior to surgery with amoxicillin, NSAIDs, and a chlorhexidine rinse. Tooth No. 8 was extracted using a flapless approach. The periapical lesion was debrided and removed separately and sent out for oral pathology evaluation. The diagnosis was confirmed as a periapical granuloma and abscess. The socket was sterilized using the ablation setting on the PerioLase® MVP-7™ laser (Millennium Dental Technologies, Inc., www.lanap.com) after vigorous use of the Piezosurgery® device (OT4 insert) (Piezosurgery Inc., www.piezosurgery.us).
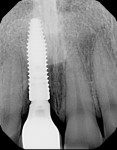
The goal was to place the implant immediately, if possible. Site preparation was done with Straumann twist drills and completed using an index finger for tactile sense along the buccal plate of bone to confirm no buccal vibration or fenestration. All socket walls were intact except the most apical buccal wall where the abscess was removed, resulting in a fenestration without a fistula. A Straumann BLT Roxolid SLActive 4.1-mm x 14-mm implant was installed using the rules for 3D placement per the ITI Treatment Guide, Volume 1.1 This was done with the aid of the anatomically correct surgical guide template—placement was along the palatal wall and in an apical position of 4 mm below the mid-facial position of the surgical guide (Figure 4). Because the coronal buccal wall was totally intact and soft tissue measured 3 mm mid-buccal, the position of the buccal implant shoulder was 1 mm deeper than the buccal height of the bone (Figure 5).
The insertion torque value of the implant was approximately 25 Ncm as it was hand-tightened to final seating. A 2-mm buccal gap was packed tightly with anorganic bovine bone (BioOss®, Geistlich Biomaterials, www.geistlich-na.com), which had been previously soaked for 10 minutes in platelet-derived growth factor (Gem-21S®, Osteohealth, www.osteohealth.com) to aid in both soft- and hard-tissue healing.
A palatal soft-tissue connective tissue graft (CTG) was harvested from the Nos. 4 and 5 site. The CTG was placed and sutured under the partially elevated buccal flap from the mesiobuccal to distobuccal line angles and, apically, approximately 10 mm to further aid in long-term soft-tissue contours. This was done to mimic the root eminence of the extracted tooth and to act as a membrane to aid in guided bone regeneration of the buccal gap (Figure 6). In addition, the CTG changed the periodontal biotype from medium to thick (ie, biotype conversion).6-8 A 7-mm tapered RC healing cap (Straumann) was placed to lightly support the soft-tissue graft and beveled to the level of the palatal tissues to prevent transmucosal loading by the tongue (Figure 6).
The dental laser was then used on the palatal incisions (hemostasis setting) to aid in bleeding control and postoperative comfort for the patient. The Essix appliance was relieved to avoid placing pressure on the surgical site. Postoperative plaque control measures were reviewed with the patient. They included normal brushing and flossing in all areas except site No. 8, where a cotton swab dipped in chlorhexidine rinse would be used to locally clean the site. The patient was also instructed to rinse with chlorhexidine twice daily until it was used completely and to finish his other medications as prescribed.
Postsurgical Follow-Up
Healing of the surgical site was uneventful, and the patient was seen at 2 weeks, 5 weeks, and 12 weeks postsurgery. A periapical x-ray was taken at 12 weeks, and a reverse torque test at 35 Ncm was completed using the manufacturer’s torque driver and RC implant carrier device to confirm bone healing. The patient was jointly scheduled with the restorative dentist for impressions to fabricate a laboratory-made screw-retained provisional restoration using the indirect method.
The patient was seen in the author’s office 3 weeks after placement of the provisional to evaluate soft-tissue healing and tissue support and for a periapical x-ray (Figure 7). Based on clinical healing and the gingival margin being slightly apical for the No. 8 implant compared to the No. 9 natural tooth, further mid-buccal support with acrylic was recommended. The adjacent papillae were healing as expected and the patient was pleased with the results at that point.9
The case was completed using the custom impression coping technique of duplication of the transitional subgingival zone for the laboratory.1,10 Because the screw-access hole in the provisional was near the palatal incisal edge, a custom abutment (with 1-mm subgingival margins circumferentially) was fabricated, and the final crown was cemented with zinc phosphate cement using the copy abutment teflon-tape technique. This technique was employed to prevent subgingival cement remnants.11
Photographs and x-rays of the final case were taken in the author’s office a few weeks after completion. The clinical examination revealed healthy soft tissues and excellent buccal contours mimicking the adjacent natural tooth (Figure 8 through Figure 11). The patient will continue periodontal maintenance visits twice yearly with his restorative dentist and annual examinations under the author’s care for 5 years to document soft- and hard-tissue healing.
Conclusion
Treatment of an esthetic zone case was successfully completed using a team approach that maximized the collaborating practitioners’ combined knowledge for the benefit of the patient.1,2,4,10 The use of the Straumann BLT Roxolid SLActive implant for immediate placement helped in the anatomical management of the central incisor site, where both the nasopalatine foramen and the normal anatomical buccal undercut can be problematic. Comprehensive case planning, the use of an anatomically correct surgical guide, evidenced-based materials—including hard- and soft-tissue grafting—along with taking the necessary time to sculpt the soft tissues in the provisional phase, are all vital to achieving a successful outcome. Because esthetic zone implant placement, as described in this case report, is a complex SAC (Straightforward, Advanced, Complex) procedure,12 surgical know-how and knowledge of the literature in this technique-sensitive area is necessary for the clinician to achieve consistently successful results, and, consequently, happy patients.
Acknowledgments
The author would like to thank George Segel, DMD, for conducting restorative therapy in the case discussed and NewTech Dental Laboratories, Inc. for its laboratory work. Dr. George Segel practices in Newtown, Pennsylvania and NewTech Dental Lab is located in Lansdale, Pennsylvania.
Disclosure
Robert A. Levine, DDS, FCPP, FISPPS, is a consultant for Straumann and Piezosurgery. He has received honorariums from ITI, Straumann, and Piezosurgery.
References
1. Buser D, Belser U, Wismeijer D, eds. ITI Treatment Guide, Vol 1: Implant Therapy in the Esthetic Zone for Single-Tooth Replacements. Berlin, Germany: Quintessence Publishing; 2007.
2. Levine RA, Nack G. Team treatment planning for the replacement of esthetic zone teeth with dental implants. Compend Contin Educ Dent. 2011;32 (4):44-50.
3. Morton D, Chen ST, Martin WC, Levine RA, Buser D. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants. 2014;29 (suppl):216-220.
4. Levine RA, Huynh-Ba G, Cochran DL. Soft tissue augmentation procedures for mucogingival defects in esthetic sites. Int J Oral Maxillofac Implants. 2014;29 (suppl):155-185.
5. Bornstein MM, Balsiger R, Sendi P, von Arx T. Morphology of the nasopalatine canal and dental implant surgery: a radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin Oral Implants Res. 2011;22(3):295-301.
6. Kan JY, Rungcharassaeng K, Morimoto T, Lozada J. Facial gingival tissue stability after connective tissue graft with single immediate tooth replacement in the esthetic zone: consecutive case report. J Oral Maxillofac Surg. 2009;67(11 suppl):40-48.
7. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-to-implant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25(2):113-119.
8. Yoshino S, Kan JY, Rungcharassaeng K, et al. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: a 1-year randomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29(2):432-440.
9. Ross SB, Pette GA, Parker WB, Hardigan P. Gingival margin changes in maxillary anterior sites after single immediate implant placement and provisionalization: a 5-year retrospective study of 47 patients. Int J Oral Maxillofac Implants. 2014;29(1):127-134.
10. Levine RA, Manji A, Faucher J, Present S. Use of titanium mesh in implant site development for restorative-driven implant placement: case report. Part 1—restorative protocol for single-tooth esthetic zone sites. Compend Contin Educ Dent. 2014;35(4):264-273.
11. Present S, Levine RA. Techniques to avoid cement around implant-retained restorations. Compend Contin Educ Dent. 2013;34(6):432-437.
12. Dawson A, Chen S. The SAC Classification in Implant Dentistry. Berlin, Germany: Quintessence Publishing; 2009.
For more information, contact:
Straumann
800-448-8168
www.straumann.us
About the Author
Robert A. Levine, DDS, FCPP, FISPPS
Clinical Professor
Department of Periodontology and Oral Implantology
Kornberg School of Dentistry, Temple University
Philadelphia, Pennsylvania
Private Practice
Pennsylvania Center for Dental Implants & Periodontics
Philadelphia, Pennsylvania